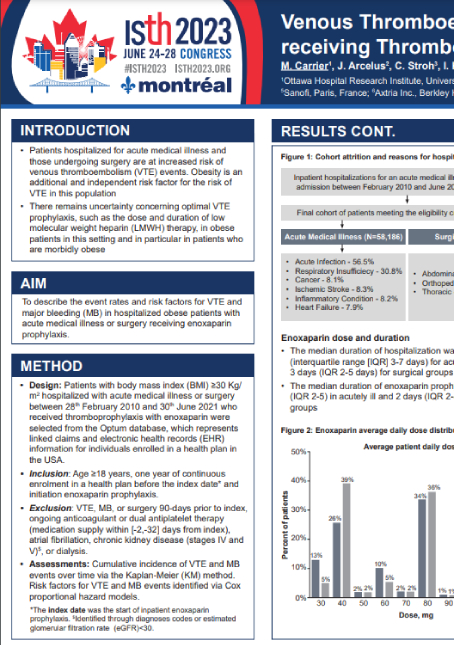
Risk Of Venous Thromboembolism And Major Bleeding In Patients With Acute Medical Illness Receiving Thromboprophylaxis With Enoxaparin
Patients hospitalized for acute medical illness and those undergoing surgery are at increased risk of venous thromboembolism (VTE). Obesity is an additional and independent risk factor for the risk of VTE in this population. Risk assessment models (RAMs) have been developed to help stratify the risk of VTE or bleeding events for individual patients; however, limited evidence exists on the patterns of risk and VTE prophylaxis in this population in contemporary usual clinical practice settings.
The objective of this study was to present descriptive analysis of a real-world population of admitted adult patients with acute medical illness initiating enoxaparin prophylaxis, including baseline clinical conditions event rates and risk factors for symptomatic VTE and major bleeding (MB). A separate analysis was later conducted on patients with obesity in medical and surgical inpatient settings.
Patients included in this study were identified in the Optum Market Clarity database from February 28, 2010, to June 30, 2021. Inclusion criteria included hospitalization for an acute medical illness (infection, respiratory insufficiency, inflammatory condition, cancer, heart failure, and ischemic stroke) with initiated enoxaparin prophylaxis, age ≥40 years old and 1-year continuous enrollment in the health plan. Exclusion criteria were VTE, MB or surgery within the previous 90 days, CKD stage IV and above, and ongoing treatment with anticoagulation or dual antiplatelet therapy. Event rates and risk factors for VTE and MB at 90-days were assessed.
The following conclusions were derived:
- There was substantial heterogeneity in the risk of VTE and MB in patients hospitalized for acute medical illness and initiated on enoxaparin. Among the subgroups, the risk of VTE varied from 3.0% in patients with ischemic stroke to 6.9% in patients with cancer-related hospitalizations, and the risk of MB varied from 1.9% in patients with inflammatory conditions to 3.6% in patients with ischemic stroke.
- Key risk factors for VTE were prior VTE (HR=4.15, 95% CI 3.80–4.53), cancer-related hospitalizations (HR=2.35, 95% CI 2.10–2.64), and thrombophilia (HR=1.64, 95% CI 1.29–2.08). Key risk factors for MB were history of MB (HR=2.17, 95% CI 1.72–2.74), history of non-MB (HR=2.46, 95% CI 2.24–2.70), and hospitalization for ischemic stroke (2.42, 95% CI 2.11–2.78).
- Risk stratification based on acute illness conditions and consideration of the full list of risk factors outlined in the study (37 conditions were significant for either VTE and/or MB event risk) may help in identification of optimal strategies for pharmacologic prophylaxis in this population.
The study was conducted with top key opinion leaders in acute medical illness and hematology, and was shared at a prestigious ISTH 2023 conference as a podium presentation. A study on the obese subpopulation was presented during the poster session.
Contact us at connect@axtria.com with any questions.
Recommended insights

Case Study
White Paper

Article